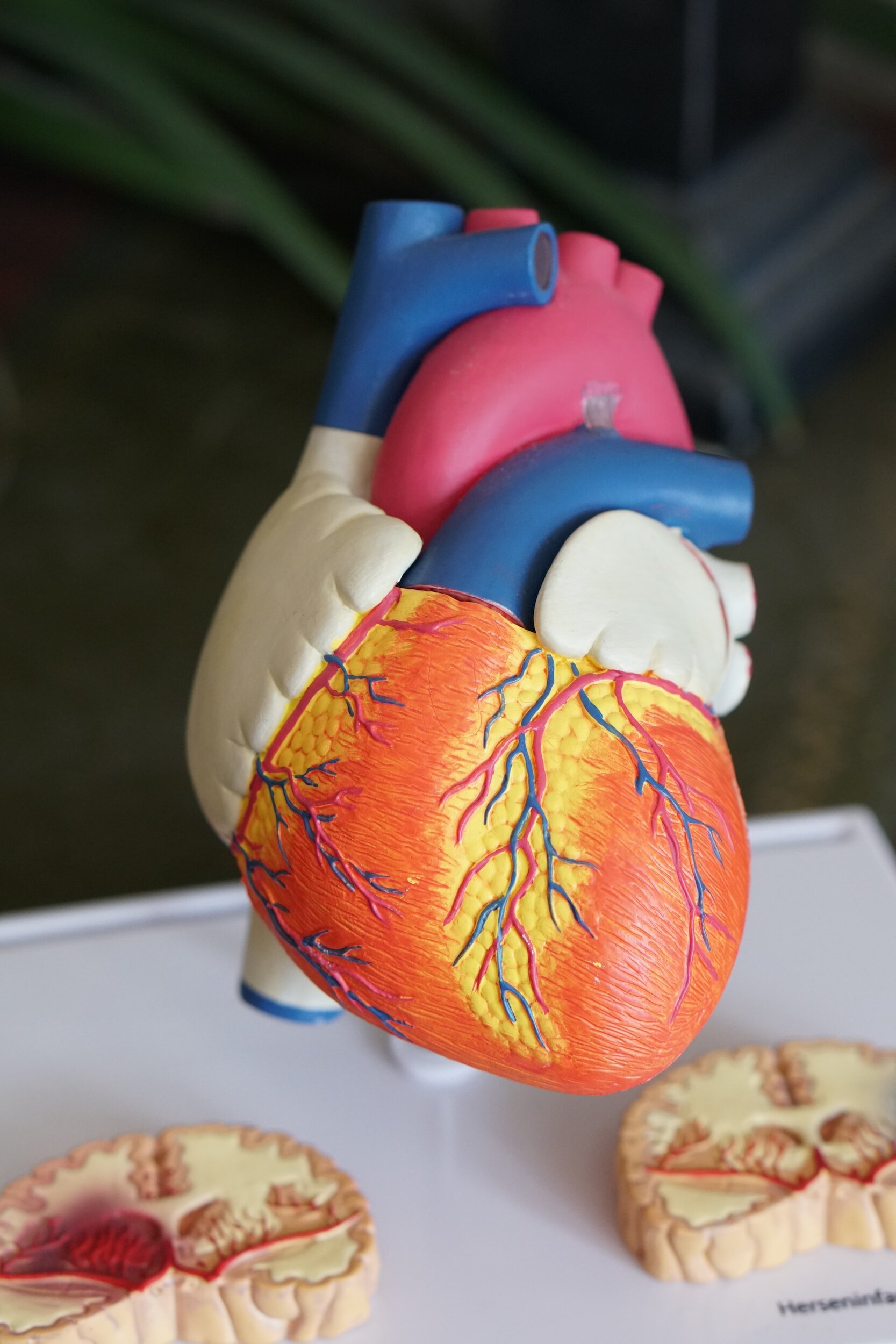
What Are Heart Valves?
Heart valves are essential components of the cardiovascular system, acting as gateways that control the flow of blood in and out of the heart. When the heart valves do not function properly, it can lead to heart valve disease. This condition occurs when there is a disruption in the normal functioning of the valves, causing them to become leaky or narrowed.
Heart valve disease can be caused by various factors, such as age, congenital defects, infections, or other medical conditions. If left untreated, heart valve disease can lead to complications like heart failure or blood clots. However, with early detection and appropriate treatment, individuals with heart valve disease can lead fulfilling and healthy lives.
Functions of Heart Valves
Heart valves play a crucial role in maintaining the proper function of the heart. These valves are responsible for ensuring one-way blood flow through the heart, preventing backward leakage and maintaining the efficiency of the cardiac cycle.
The heart has four valves: the mitral valve, tricuspid valve, aortic valve, and pulmonary valve. Depending on which part of the heart is contracting or relaxing, they either open or close to allow blood to flow forward in one direction. This ensures that blood is directed towards the body or through the pulmonary artery to the lungs, depending on the valve, without any backward leakage.
Any abnormalities or malfunctions in these valves can lead to heart valve diseases, which may require medical intervention or surgical treatment to restore normal functioning.
Symptoms of Heart Valve Diseases
Heart valve disease occurs when one or more of the heart valves are damaged or not functioning properly. Common symptoms of heart valve disease may vary depending on the specific valve affected and the severity of the disease.
Chest Pain
Chest pain can be a symptom of heart valve disease. As the heart needs to work harder to keep blood flowing smoothly forward, this can result in chest pain if the blood supply to the heart is not optimal, or the valve is severely affected.
Several factors can trigger or exacerbate chest pain related to heart valve issues. Physical exertion, emotional stress, or certain medications can increase the workload on the heart, leading to chest pain. Additionally, a buildup of blood clots or increased blood pressure in the heart can also cause chest pain.
If an individual experiences chest pain, it is important to seek immediate medical attention. Chest pain can be a sign of a potentially life-threatening condition, and it is essential to receive a proper diagnosis and treatment. Medical professionals can perform various tests, such as a chest x-ray or blood tests, to evaluate the heart and identify any underlying heart valve issues. Seeking prompt medical attention can help prevent further complications and improve outcomes for individuals with heart valve diseases.
Shortness of Breath
Shortness of breath is one of the common symptoms experienced by individuals with heart valve diseases. It occurs when the heart valves are not functioning properly, leading to impaired blood flow throughout the body. As a result, the body may not receive an adequate supply of oxygen, causing difficulty in breathing.
Valve disorders such as regurgitation and stenosis can contribute to shortness of breath. Regurgitation occurs when a valve fails to close completely, causing blood to flow backward. This places extra strain on the heart, making it harder to pump blood efficiently. Stenosis, on the other hand, happens when a valve becomes narrow or constricted, limiting the amount of blood that can flow through. This reduced blood flow can result in decreased oxygen supply to the body’s tissues and organs, including the lungs, leading to shortness of breath.
Several causes can contribute to shortness of breath in individuals with valvular heart diseases. Physical exertion or even mild activities can trigger breathlessness due to the heart’s decreased ability to pump blood effectively. Increased pressure in the heart can also cause fluid to accumulate in the lungs, further contributing to difficulty in breathing.
Treatment options for alleviating shortness of breath caused by heart valve conditions depend on the severity and type of valve disorder. Medications can be prescribed to manage symptoms and improve heart function. In more severe cases, surgery may be necessary to repair or replace the damaged valve. Lifestyle changes such as maintaining a healthy weight, quitting smoking, and managing stress can also help manage symptoms and improve overall heart health.
If you are experiencing shortness of breath or other symptoms related to heart valve diseases, it is crucial to seek medical attention promptly to receive an accurate diagnosis and appropriate treatment.
Fatigue and Weakness
Fatigue and weakness are common symptoms experienced by individuals with heart valve diseases. These conditions can significantly impact a person’s quality of life, making routine activities more difficult to perform.
Regular check-ups and monitoring are crucial for individuals with heart valve diseases. Changes in symptoms, such as increased fatigue and weakness, should be promptly reported to a healthcare professional. Regular follow-ups allow for the assessment of the condition’s progression and adjustment of treatment plans as needed.

Swelling in the Feet, Ankles, and Legs
Swelling in the feet, ankles, and legs can be a common symptom associated with heart valve diseases. When the heart valve fails to function properly, it can lead to fluid buildup in the body, a condition known as oedema. This excess fluid can accumulate in the lower extremities, causing swelling.
Valve problems can disrupt the normal flow of blood, leading to increased pressure within the blood vessels. This increased pressure can cause fluid to leak out of the blood vessels and into the surrounding tissues, resulting in swelling.
In addition to swelling in the feet, ankles, and legs, other symptoms may also be present. These can include a swollen abdomen, breathing difficulties, fatigue, and a rapid or irregular heartbeat.
If the swelling is mild and not significantly impacting the individual, the doctor may choose to closely monitor the condition before deciding on treatment. However, it is important to report any changes or worsening of symptoms to a healthcare professional. Regular check-ups and follow-ups are crucial for the proper management of heart valve diseases, as well as to monitor and address any fluid buildup that may occur.
If you experience persistent or severe swelling, it is important to seek medical attention, as this could indicate a potential complication of heart valve disease.
Irregular Heartbeat (Arrhythmia)
Heart valve diseases can be associated with various types of irregular heartbeat, also known as arrhythmia. Arrhythmia occurs when there is a disruption in the normal electrical signals that regulate the heart’s rhythm.
Valve abnormalities, such as stenosis or regurgitation, can interfere with the heart’s electrical system and lead to arrhythmias. The irregular blood flow caused by faulty valves can create extra strain on the heart, triggering abnormal heartbeats.
Symptoms of arrhythmias include:
– A rapid or irregular heartbeat
– Palpitations
– Chest discomfort
– Dizziness
– Shortness of breath
– Fainting.
These symptoms should not be ignored, as they could be a sign of an underlying heart condition, including valvular disease.
It is crucial to seek medical attention if any irregular heartbeats are experienced, as early detection and treatment of heart valve diseases can help prevent complications such as heart failure or blood clots. Your doctor may recommend diagnostic tests such as an echocardiogram or a cardiac catheterisation to assess the severity of the valve disorder and determine the most appropriate treatment plan.
If you are experiencing any symptoms of arrhythmia or suspect you may have a heart valve problem, it is important to consult a healthcare professional for an accurate diagnosis and appropriate management of your condition.
Dizziness or Fainting
Heart valve diseases can cause symptoms such as dizziness or fainting. These symptoms occur due to reduced blood flow and abnormal heart rhythm caused by valve abnormalities.
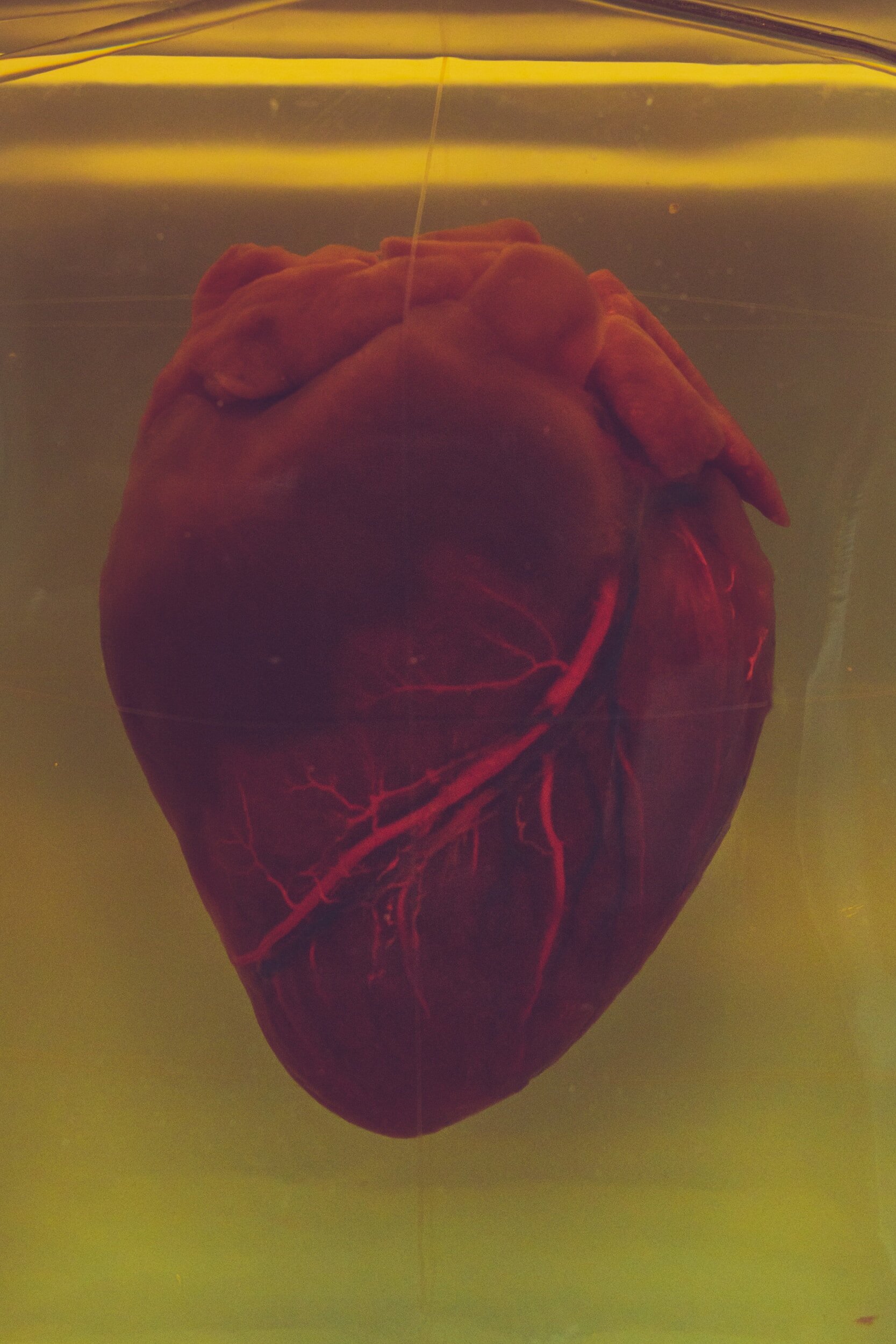
Types of Heart Valve Diseases
There are multiple different types of valve disease within the heart. The causes can vary, with some cases being congenital or present at birth. Other causes include infective endocarditis, rheumatic fever, heart attacks, ageing, and degenerative conditions.
In this next section we will provide an overview of the most common types of heart disease and their causes.
Stenosis vs. Regurgitation
Stenosis and regurgitation are two common types of valve malfunctions that occur in heart valve diseases. Understanding the difference between these conditions is important in diagnosing and treating patients effectively.
Stenosis occurs when a heart valve is unable to fully open, resulting in restricted blood flow. This narrowing of the valve can be caused by factors such as calcium deposits, scarring, or congenital defects. In the case of stenosis, the affected valve does not open properly, making it difficult for blood to flow through. This can lead to symptoms like chest pain, fatigue, and shortness of breath.
On the other hand, regurgitation is where you have a leaky valve. This happens when a heart valve leaks and blood flows backward. This occurs when the valve fails to close tightly, allowing blood to flow back into the chamber it came from. Regurgitation can be caused by factors such as valve damage from infections or congenital abnormalities. Symptoms of regurgitation can include fatigue, heart palpitations, and shortness of breath.
In the context of heart valve diseases, mitral valve stenosis is a common condition, often caused by rheumatic heart disease. In the UK this condition has been almost eradicated through the widespread use of antibiotics. As a result the number of people diagnosed with mitral stenosis has decreased. Rheumatic heart disease is an inflammatory condition that can develop after an infection with streptococcal bacteria, commonly called strep throat. Over time, this condition can cause scarring and narrowing of the mitral valve, leading to mitral stenosis.
Mitral Valve Stenosis
Mitral Valve Stenosis is a common type of heart valve disease where the mitral valve does not open properly. This can cause a narrowing in the blood flow, leading to symptoms such as chest pain, fatigue, and shortness of breath. The most common cause of Mitral Valve Stenosis is rheumatic heart disease, an inflammatory condition that develops after an infection with stre ptococcal bacteria. Other causes of Mitral Valve Stenosis include infection, scarring, calcium deposits, and congenital defects. Treatment options can range from medications to open the valve or surgical interventions to repair or replace it.
Aortic Regurgitation
Aortic Regurgitation is another type of heart valve disease where the aortic valve does not close properly, resulting in a leaky valve. This allows blood to flow back into the left ventricle, resulting in an abnormal backward flow of oxygen-rich blood. Aortic regurgitation can be caused by factors such as infection, ageing, high blood pressure, or congenital defects. Symptoms of aortic regurgitation can include palpitations, chest pain, fatigue, and shortness of breath. Treatment options can range from medications to open the valve or surgical interventions to repair or replace it.
Aortic Stenosis
Aortic stenosis is the more common heart valve diseases. This causes outflow obstruction in the left ventricle and can be the result of ageing or congenital abnormalities, such as bicuspid aortic valves (a birth defect where there is an abnormal structure of the aortic valve). This condition occurs when the aortic valve becomes narrowed, preventing the normal flow of blood from the heart’s left ventricle to the rest of the body.
There are several possible causes of aortic valve stenosis and regurgitation. One common cause is the natural wear and tear of ageing, where the valve becomes stiff and calcium deposits build up, leading to narrowing and restricted blood flow.
In addition to ageing and congenital abnormalities, aortic stenosis can also occur due to other factors, including aortic dissection (a tear in the aortic wall), trauma, certain diseases like rheumatic fever, and infections such as infective endocarditis.
Treatments for aortic stenosis include medications, lifestyle modifications and aortic valve replacement.
Tricuspid Regurgitation
Tricuspid regurgitation is a condition where the tricuspid valve in the heart does not close properly, leading to a backflow of blood into the right atrium from the right ventricle. This can result in a number of symptoms and signs, particularly those related to right-sided heart failure.
One common symptom of tricuspid regurgitation is ascites, which refers to the accumulation of fluid in the abdominal cavity. This can cause abdominal swelling and discomfort. Another sign of right-sided heart failure is hepatomegaly, or an enlarged liver, due to the increased pressure in the liver’s blood vessels.
Jugular venous distension is also commonly observed in tricuspid regurgitation. The backflow of blood can lead to an increase in jugular venous pressure, causing the veins in the neck to become visibly dilated.
Mitral Regurgitation
Mitral valve regurgitation is a condition where blood flows in the wrong direction in the heart due to a faulty mitral valve. The mitral valve separates the left atrium from the left ventricle and is responsible for preventing the backflow of blood during heart contractions. There are several causes of mitral regurgitation, including normal ageing, heart attack, heart infections, rheumatic fever, and mitral valve prolapse.
Symptoms of mitral regurgitation may include fatigue, shortness of breath, and fluid retention, which can lead to swelling in the legs and ankles. In severe cases, it can result in heart failure. It is more commonly found in older individuals, with a prevalence rate of approximately 10% in those aged 75 and above. Normal ageing can contribute to the development of mitral regurgitation as the valve becomes less flexible and may leak blood backward. People who suffer with a connective tissue disorder are also at higher risk of developing this condition.
Treatment options for mitral regurgitation often depend on the severity of the condition. Medications may be prescribed to manage symptoms and help the heart function more efficiently. In some cases, surgical intervention, such as valve repair or replacement, may be necessary. Valve replacement options include mechanical valves, which are long-lasting but require long-term blood-thinning medication, and biological valves, which do not require blood-thinning medication but have a limited lifespan.

Where to Find Support or More Information
If you or someone you know is seeking support or more information regarding heart valve diseases, there are various resources available to help. The British Heart Foundation (BHF) is a reliable source and offers comprehensive information and support on heart valve disease. Their website provides in-depth articles, videos, and downloadable resources for individuals to learn about heart valve diseases, their causes, symptoms, and treatment options.
It is important to consult with healthcare professionals for personalised advice and treatment options. However, finding reliable and accurate information from trusted sources such as the BHF and other reputable organisations can empower individuals to make informed decisions about their health and well-being.
FAQs
I suffer with breathlessness and dizziness; could it be heart valve disease?
There are many causes of breathlessness and dizziness. What is most likely to be causing individuals symptoms will depend on the person in question. For example, a young woman who is otherwise healthy presenting with these symptoms would be more likely to be suffering from iron deficiency anaemia than diseases of the heart valves. If you were to visit your GP they would take a history and may do a physical examination, this will result in further tests being ordered to look for the possible causes of your symptoms. It is important to see a GP if you are concerned about symptoms like this or those mentioned elsewhere in this article.
What kind of tests might my GP send me for?
If you were to present to your GP with concerns about your heart or symptoms as described in this article they will take a thorough medical history. Following this a number of tests might be ordered. These may include:
– Listening to your heart: A heart murmur may be heard when listening to your heart sounds.
– Blood tests: These will be done to look for other causes of breathlessness such as kidney disease or anaemia. Certain blood tests can also be done to check for heart failure (a BNP level).
– ECG: This may be a one off trace of your heart, or if you are complaining of palpitations it may be a monitor that you wear over 24 hours to a week to make sure your heart isn’t occasionally having abnormal rhythms.
– Blood pressure: Again this may be a one off measurement during your consultation or a monitor applied to your arm over a 24 hour period which you can wear at home and periodically checks your blood pressure throughout the day.
– Lying standing blood pressures: Comparing your blood pressure when you lie down to when you stand up. A big drop may be the cause of your dizziness.
– An ECHO: This is an ultrasound scan of your heart which can measure how well it is functioning and assess the valves and blood flow.
– Coronary angiogram: This scan looks for coronary artery disease. If you are presenting with periods of chest pain this might be done to look at the blood vessels that supply blood to the heart walls. When these become narrowed this can cause chest pain that may be due to angina or even heart attacks.
Can diseases of heart valves lead to heart failure?
Diseases of heart valves, if left untreated, can progress and lead to heart failure. It is important if you are diagnosed with any heart conditions to follow recommendations from your health care provider.
Can I have a valve replacement without open heart surgery?
Yes, in certain cases, a valve replacement can be done without open heart surgery. This is more commonly done in aortic valve replacement. In this procedure, a catheter (a thin tube inserted into a vein) is used to guide the new valve to its correct location within the heart. This can be a less invasive procedure than open heart valve surgery, but it is important to remember that not everyone will be suitable for this type of surgery. If you are considering whether to have this surgery it is best to discuss the pros and cons with your cardiologist.


