Head injuries presenting to Emergency Departments can range from alarming medical situations that require immediate assessment and intervention, to minor bumps that require only reassurance and advice. Deciding when to perform scans is made much simpler by clear algorithmic approaches, such as those recommended by the National Institute for Health and Care Excellence (NICE) guidelines on head injury.
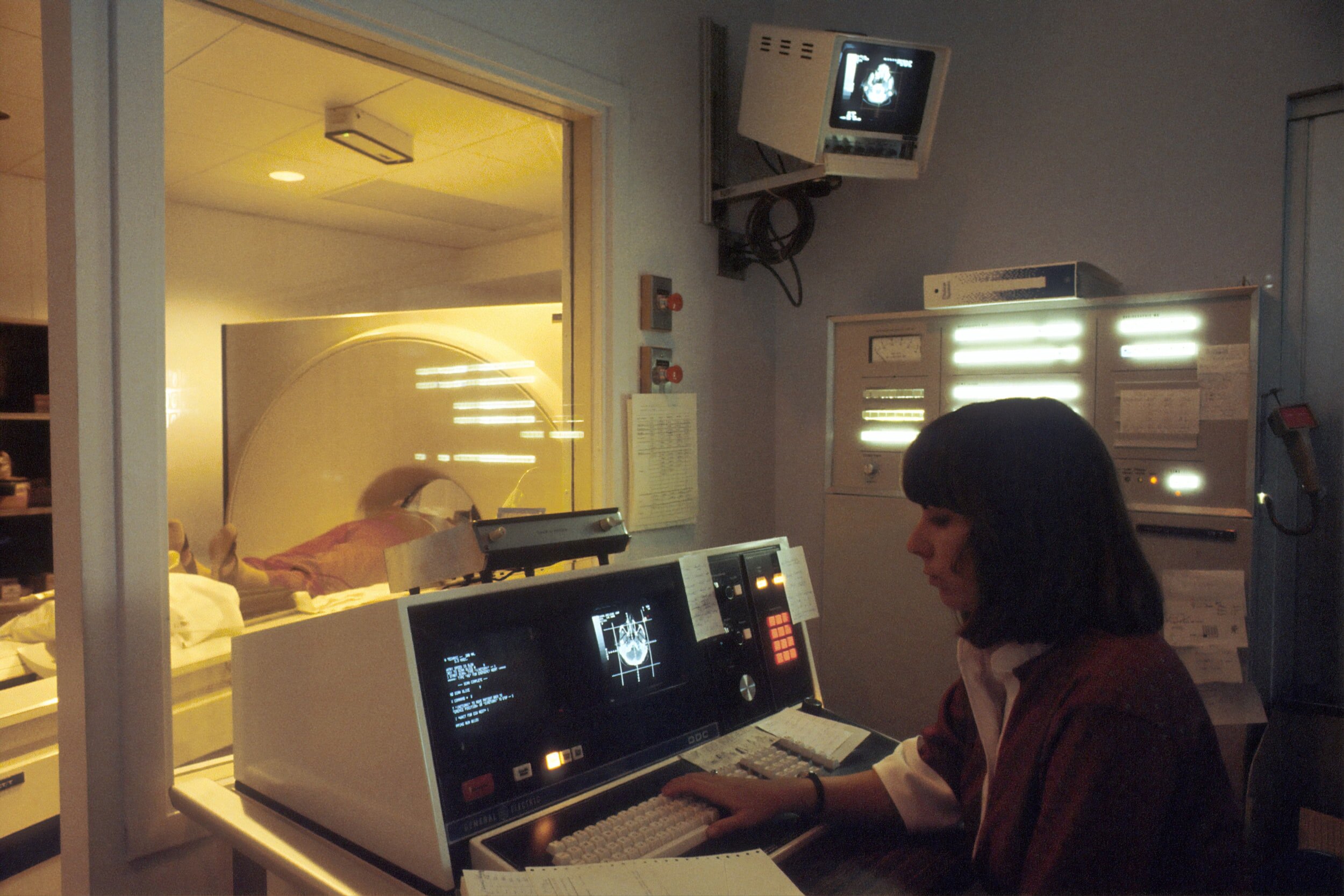
As emergency medicine continues to evolve, computed tomography (CT) scans have become a cornerstone in the evaluation of adult patients with head injuries. However, the question of when to perform a CT scan often depends on several factors such as the severity of the injury, the patient’s symptoms, and potential risks. This article, leveraging insights from NICE, aims to provide a comprehensive review of when a CT scan is recommended for an adult with a head injury.
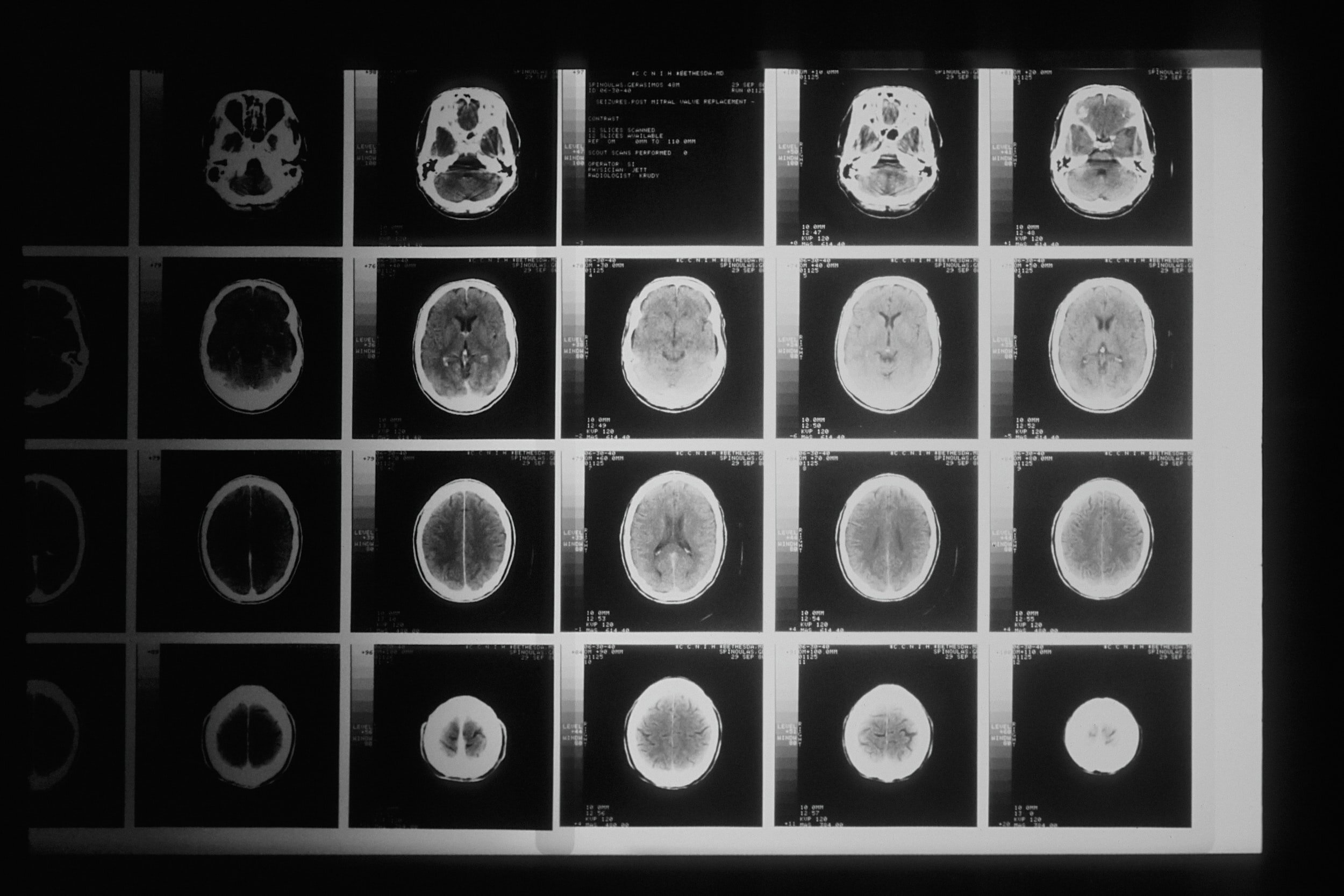
Understanding the Role of a CT Scan
A CT scan is a non-invasive diagnostic tool that uses X-rays to generate a detailed image of the brain, providing a vital perspective on any potential intracranial injuries or abnormalities. The scan can reveal brain bleeds, fractures, contusions (bruising), or swelling, which are crucial in determining the right treatment plan.
While the CT scan is an invaluable tool, it is not without risks. One key consideration is the exposure to ionising radiation, which can potentially increase the risk of cancer. Hence, the benefits and risks must be balanced, with the CT scan only used when clearly indicated.
NICE CT Head Guidance
The National Institute for Health and Care Excellence (NICE) has provided a robust set of guidelines, often seen as the gold standard in the UK, for when to conduct a CT scan in an adult who has suffered a head injury.
Firstly, an immediate CT scan is recommended in adults who have suffered a head injury and present with any of the following symptoms:
- A Glasgow Coma Scale (GCS) score less than 13 upon initial assessment.
- A GCS score less than 15 at 2 hours after the injury.
- Boggy swellings or palpable dips in the skull suggestive of depressed skull fractures.
- Signs of fractures of the base of the skull including; blood behind the ears (haemotympanum), ‘panda’ eyes, clear fluid leaking from the ears or nose, or bruising behind the ears.
- Post-traumatic seizure.
- Focal neurological signs (such as weakness, visual or sensory disturbance etc).
- More than one episode of vomiting.
If none of the above are present, but an adult who has had some loss of consciousness or amnesia since the injury presents, perform a CT head scan within 8 hours of the head injury if they have any of the following risk factors:
- Age 65 or over.
- Any current bleeding or clotting disorders (including being on blood thinning medications)
- Dangerous mechanism of injury.
- More than 30 minutes’ retrograde amnesia.
NB. In practice all patients who are on anticoagulants and present to Emergency departments with head injury get a CT head. There has been a recent move to include antiplatelets, including aspirin and clopidogrel, as an indication for a CT head also.

Important Considerations for CT Head Decision-Making
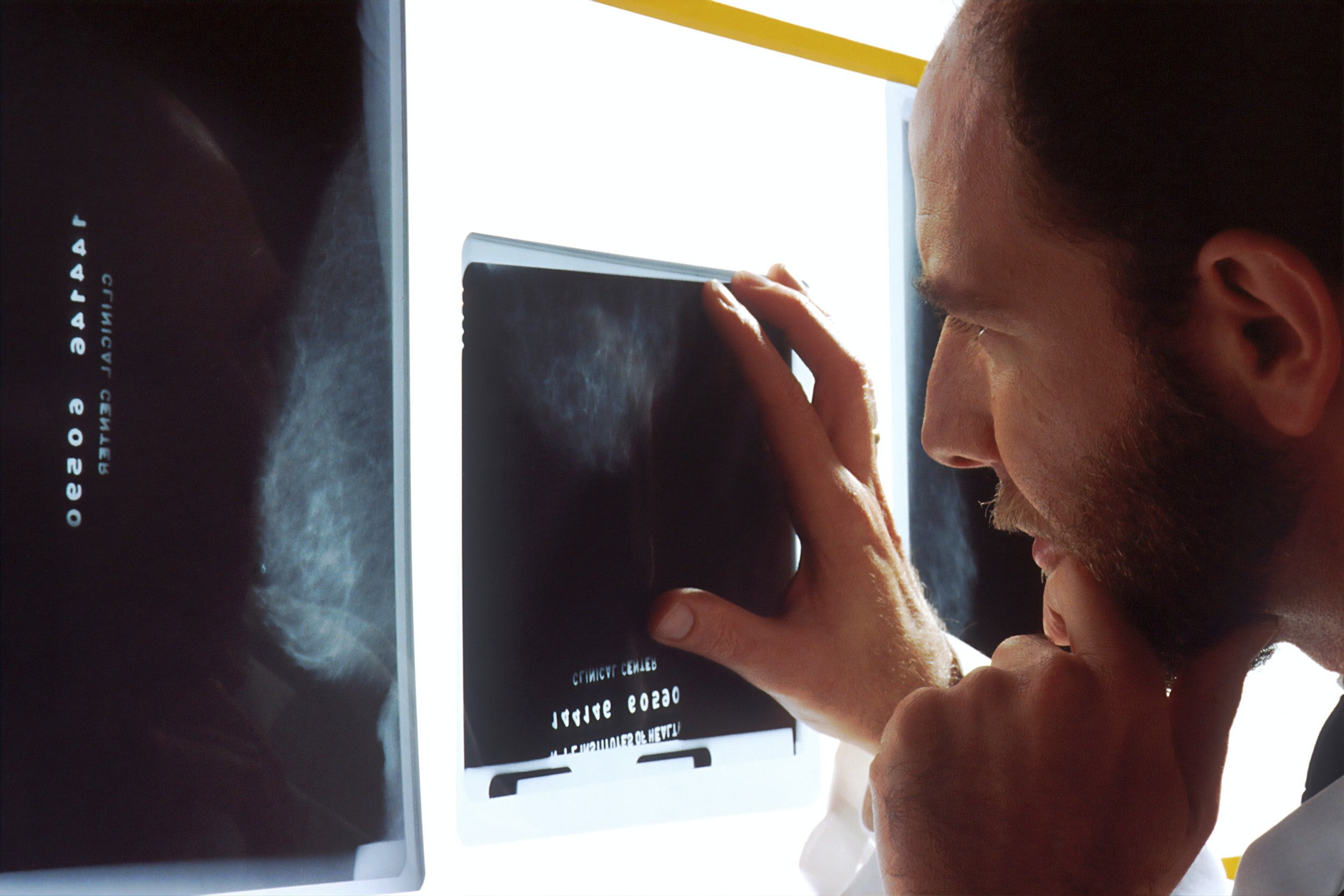
Each patient and head injury is unique, requiring careful assessment. Consider the mechanism of injury, the patient’s clinical presentation, and any underlying medical conditions when deciding on the need for a CT scan. Always prioritise patient safety and aim to prevent secondary injuries from delayed or missed diagnoses.
There are some key factors that could influence this decision-making process:
- Patient’s Age: Older adults (65 years and above) are more likely to suffer significant injuries from minor head trauma due to their increased vulnerability. Moreover, they are at a higher risk of intracranial bleeding, especially if they are on anticoagulation therapy.
- Mechanism of Injury: The cause of the injury plays a crucial role in decision-making. High-risk mechanisms such as falls from height, high-speed motor vehicle collisions, or assaults are more likely to result in serious head injuries.
- Clinical Symptoms: The presence of any neurological symptoms or signs, including confusion, seizures, severe headache, repeated vomiting, or visual problems, warrants a CT scan.
- Medical History: Patients with a history of coagulopathies or those on anticoagulants are more prone to bleeding, necessitating a CT scan after head injury, even if there are no initial symptoms.
- Intoxication: Never assume confusion or other concerning symptoms are due to alcohol or drugs in those presenting as intoxicated. If there is a head injury and they meet any of the criteria above always do a CT.
Remember, these are not rigid rules, but guidelines to aid in decision-making. Clinicians should use their judgment and clinical experience to decide the best course of action for each patient.
CT Scans: Not Always Necessary
It’s important to emphasise that not every head injury requires a CT scan. Many minor injuries can be safely managed without scanning. This is why understanding the criteria for conducting a CT scan is essential – it allows for prudent use of resources, reduces unnecessary radiation exposure, and helps to avoid overcrowding in emergency departments.
For minor injuries where the NICE guidelines do not indicate the need for a CT scan, observational management can be an effective approach. The patient can be closely monitored, and if their condition deteriorates or they develop symptoms indicating a more serious injury, a CT scan can be performed at that point.
The Future of Head Injury Assessment
With advancements in technology and medical research, new assessment tools are emerging. For example, blood tests that identify brain injury markers could potentially reduce the need for CT scans in the future. These are, however, still in the early stages of development and require further research and validation.
Similarly, clinical decision rules such as the Canadian CT Head Rule and the New Orleans Criteria have been developed to help clinicians decide when to use CT scanning in minor head injury. They are validated tools, and their use can lead to a reduction in unnecessary CT scans.
Conclusion
While CT scans play an indispensable role in the evaluation and management of head injuries in adults, knowing when to use them is crucial. Head injury guidelines provided by NICE form a strong foundation for making these important clinical decisions. As medical science advances, we can look forward to even more precise and patient-friendly strategies in the management of head injuries. To access the full NICE CT head guidance, visit this page.


