Diabetes is a prevalent and challenging medical condition that affects millions worldwide. It is characterised by high levels of glucose (sugar) in the blood, which if left untreated can lead to severe health complications.
In this article, we aim to provide a comprehensive understanding of what diabetes is, including its types, primary causes, symptoms, and potential complications. Additionally, we will explore modern methods of diabetes management, such as lifestyle modifications, medication, and innovative therapeutic approaches that can help achieve optimal blood sugar levels.
Furthermore, we believe it is essential to dispel common misconceptions about diabetes and highlight the significance of early detection and regular monitoring for maintaining a healthy and fulfilling life.
An Overview of What Diabetes Is
To comprehend diabetes, it’s crucial to understand what occurs in our bodies when we consume food. After eating carbohydrates, our body breaks them down into glucose, which enters the bloodstream. Insulin, a hormone produced by the pancreas, regulates the amount of glucose in the blood by directing it to our cells to be used as energy.
Diabetes is a condition that arises when this process malfunctions. There are two primary types of diabetes: Type 1 and Type 2.
What is Diabetes Type 1
Diabetes Type 1 is a chronic condition that occurs when the pancreas either does not produce enough insulin or stops producing it altogether.
Type 1 diabetes is an autoimmune disease where the immune system attacks and destroys the insulin-producing beta cells in the pancreas, resulting in high blood sugar levels. Individuals with Type 1 diabetes must inject insulin daily to regulate their blood sugar levels. Common symptoms of Type 1 diabetes include:
- Frequent urination
- Increased thirst and hunger
- Unexplained weight loss
- Blurred vision
- Fatigue
What is Diabetes Type 2?
On the other hand, Diabetes Type 2 is a metabolic condition that occurs when the body becomes resistant to insulin, causing glucose to accumulate in the bloodstream instead of being absorbed by cells.
While Type 2 diabetes typically affects adults over the age of 40, it can occur at any age. It may be caused by various factors such as genetics, obesity, sedentary lifestyle, and poor diet. Common symptoms of Type 2 diabetes include:
- Frequent urination
- Increased thirst and hunger
- Blurred vision
- Fatigue
- Flow-healing wounds
However, some people with Type 2 diabetes may not experience any initial symptoms, making diagnosis challenging. For more information on diagnosing diabetes, read our comprehensive article on the WHO diabetes diagnostic criteria.

The Key Differences Between Type 1 and Type 2 Diabetes
In both Type 1 and Type 2 diabetes, high blood sugar levels can lead to serious health complications like nerve damage, kidney damage, and vision problems. Thus, early diagnosis and management are crucial to preventing long-term health consequences.
There are, however, some notable differences between diabetes Type 1 and diabetes Type 2, which have been summarised below:
- Type 1 diabetes is an autoimmune disease that causes the body to stop producing insulin, while type 2 diabetes is when the body cannot use insulin effectively.
- Type 1 diabetes usually develops in childhood, whereas type 2 diabetes is more common in adults.
- People with type 1 diabetes require insulin therapy, while those with type 2 diabetes can often manage their condition through healthy lifestyle changes, medication, and/or insulin therapy.
- Type 1 diabetes is considered more severe than type 2 diabetes and can lead to serious complications, including vision loss, kidney damage, and nerve damage.
- Type 2 diabetes is associated with several risk factors, including obesity, physical inactivity, and a poor diet, while the cause of type 1 diabetes is not yet fully understood.
- While both types of diabetes can cause high blood sugar levels, the symptoms of type 1 diabetes often develop more quickly and are more severe than those of type 2 diabetes.
- Type 2 diabetes is much more prevalent than type 1 diabetes, accounting for about 90% of all cases of diabetes worldwide. Type 1 diabetes accounts for only about 5-10% of cases.
How Diabetes is Treated
Managing diabetes is key for maintaining good health. Here’s an overview of how diabetes can be treated:
- Insulin therapy: People with Type 1 diabetes require insulin therapy, and some people with Type 2 diabetes may also need insulin if other treatments are not effective in controlling blood sugar levels.
- Oral medications: Medications such as metformin, sulfonylureas, meglitinides, DPP-4 inhibitors, GLP-1 receptor agonists, and SGLT2 inhibitors can help manage blood sugar levels by either increasing insulin production or reducing glucose absorption from the digestive system.
- Lifestyle changes: Dietary modifications, such as reducing sugar and carbohydrate intake, and incorporating more whole grains, vegetables, and fruits into meals can help control blood sugar levels. Regular exercise is also important in managing diabetes.
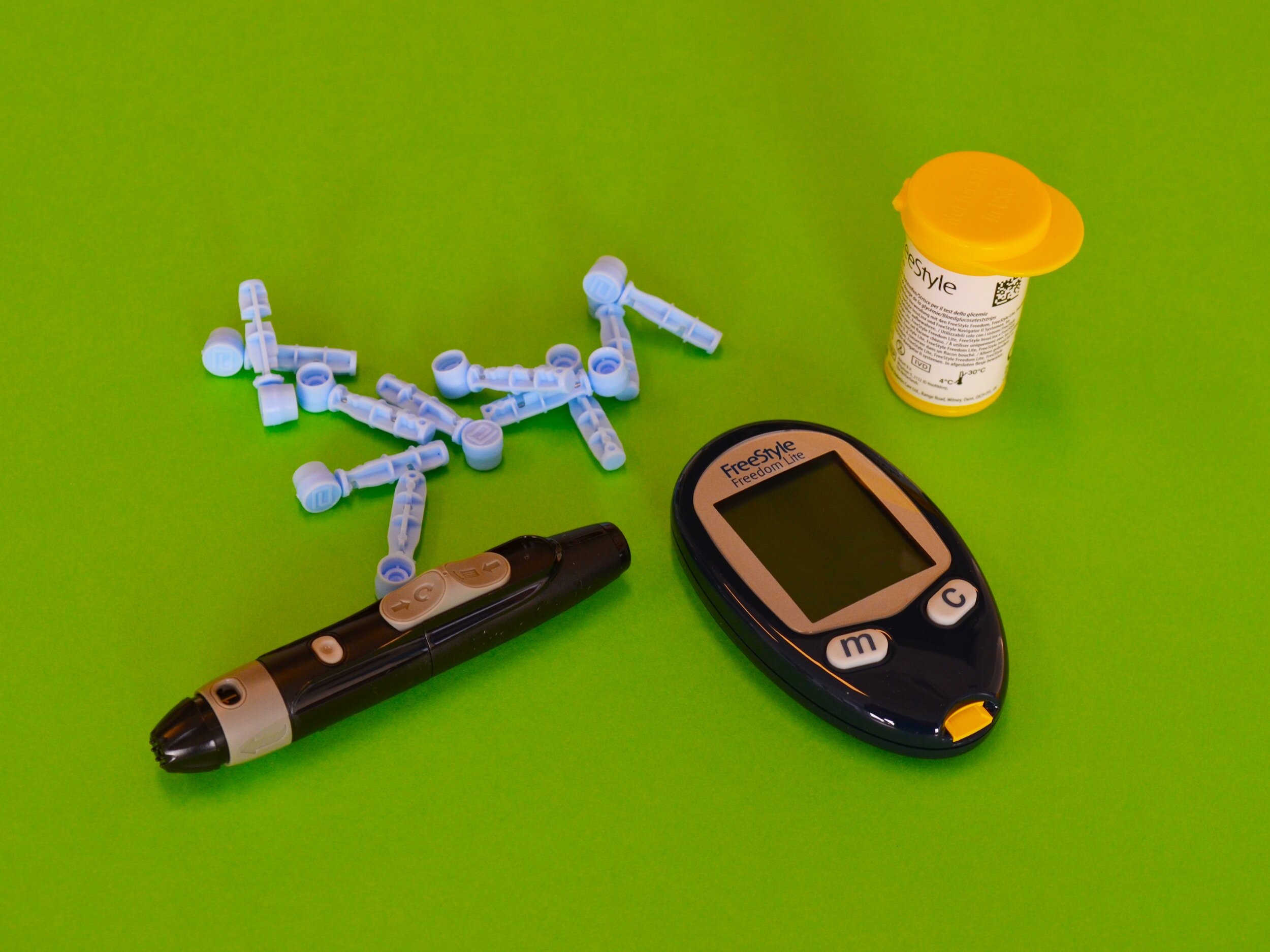
- Blood sugar monitoring: Regular monitoring of blood sugar levels is crucial in managing diabetes. This can be done at home using a blood glucose meter.
- Weight management: Maintaining a healthy weight can help reduce the risk of developing Type 2 diabetes and help manage existing diabetes.
- Regular medical check-ups: Regular medical check-ups, including blood sugar tests, blood pressure checks, and cholesterol tests, are important for managing diabetes and preventing complications.
- Bariatric surgery: In some cases, bariatric surgery may be recommended for people with severe obesity and Type 2 diabetes to help improve blood sugar control.
- Alternative therapies: Some people with diabetes may benefit from complementary and alternative therapies, such as acupuncture, yoga, or herbal supplements. However, these interventions should be used in conjunction with traditional treatments and under the guidance of a healthcare provider.

Common Diabetes Questions
How Many Diabetes Types Are There?
There are three main types of diabetes: Type 1, Type 2, and gestational diabetes. As we’ve explored in this article, Type 1 diabetes is caused by an autoimmune reaction that destroys insulin-producing cells in the pancreas and Type 2 diabetes occurs when the body becomes resistant to insulin or does not produce enough insulin to maintain normal blood sugar levels.
Gestational diabetes develops during pregnancy and usually goes away after the baby is born, although it increases the risk of developing Type 2 diabetes later in life. It’s important to note that there are other rarer forms of diabetes, such as monogenic diabetes and cystic fibrosis-related diabetes, but they account for a small fraction of all diabetes cases. Understanding the different types of diabetes is essential in managing the condition effectively and preventing complications.
Can Diabetes Be Reversed?
According recent research, Type 2 diabetes cannot be cured, but individuals can have glucose levels that return to non-diabetes range (complete remission) or pre-diabetes glucose level (partial remission).
The primary means by which people with Type 2 diabetes achieve remission is by losing significant amounts of weight through diet and exercise. Losing as little as 5-10% of body weight can improve blood sugar control and potentially even lead to remission in some cases. Maintaining a healthy weight, engaging in regular physical activity, and following a healthy diet are crucial in managing diabetes effectively. While Type 1 diabetes cannot be reversed, proper management can help individuals live healthy and fulfilling lives.
Can Diabetes Kill You?
Untreated diabetes can indeed lead to serious complications and, ultimately, death. Over time, high blood sugar levels can damage blood vessels and nerves throughout the body, leading to a range of health problems including heart disease, stroke, kidney failure, nerve damage, eye damage or blindness, dental disease, skin conditions, and slow wound healing.
Additionally, people with diabetes are at increased risk for infections, mental health issues, and other complications. However, with proper management of blood sugar levels and regular medical care, many of these complications can be prevented or delayed, and individuals with diabetes can lead long, healthy lives.
It’s essential to work with a healthcare team to manage diabetes effectively, which may include monitoring blood sugar levels, taking medications as prescribed, following a healthy diet, exercising regularly, and staying up-to-date on recommended preventive care screenings.
Which Diabetes Is Worse?
Type 1 and type 2 diabetes are both serious health conditions that need to be managed carefully and can lead to significant health complications if not well-controlled. While there is no definitive answer as to which diabetes is worse, each has its own unique challenges and risks. Ultimately, both types of diabetes require careful management to prevent complications and maintain long-term health.
Can Diabetes Cause Headaches?
High or low blood sugar levels in people with diabetes can trigger headaches. Headaches caused by high blood sugar tend to be dull and throbbing, and can occur as a result of diabetic ketoacidosis (DKA), a dangerous complication of uncontrolled diabetes.
DKA occurs when the body breaks down fat for energy instead of glucose, leading to high levels of ketones in the blood. Ketones can cause dehydration, which can lead to symptoms such as headache, nausea, and fatigue. Additionally, low blood sugar levels can also cause headaches in people with diabetes.
Hypoglycaemia, or low blood sugar, can occur as a result of taking too much insulin or other diabetes medications, skipping meals, or engaging in strenuous physical activity without adequate fuel. Headaches caused by hypoglycaemia may feel dull or throbbing and typically improve once blood sugar levels return to normal.

Which Diabetes Is Genetic?
Type 2 diabetes is the type of diabetes that has a strong genetic component. While lifestyle factors such as obesity and physical inactivity also play a role in the development of Type 2 diabetes, research has shown that genetics can increase an individual’s risk of developing the condition.
In fact, having a family history of Type 2 diabetes is one of the most significant risk factors for the disease. Studies have identified several genes that are associated with an increased risk of Type 2 diabetes, including genes involved in insulin secretion, insulin resistance, and glucose metabolism. However, it’s important to note that genetics alone do not cause Type 2 diabetes, and lifestyle factors such as diet, exercise, and weight management also play a crucial role in its development and management.
Can Diabetes Cause High Blood Pressure?
According to several reliable sources, including Johns Hopkins Medicine and the American Diabetes Association, people with diabetes are at increased risk for developing high blood pressure (hypertension). Hypertension is a common comorbidity of diabetes, with up to 60% of people with diabetes also having hypertension.
While the exact link between diabetes and high blood pressure is not fully understood, research suggests that insulin resistance and endothelial dysfunction (damage to the lining of blood vessels) may play a role. Additionally, lifestyle factors that increase the risk of developing Type 2 diabetes, such as obesity, physical inactivity, and poor diet, also increase the risk of developing high blood pressure.
It’s important for people with diabetes to monitor their blood pressure regularly and work with their healthcare team to manage both conditions effectively through lifestyle changes, medications, and other treatments as needed.
Can Diabetes Cause Dizziness?
In people with diabetes, dizziness is one of the symptoms that can happen due to high blood glucose levels. The level of dizziness can vary, from mild lightheadedness to feeling like the ground beneath you is tilting. Some describe the experience as if their head is spinning, even though they’re standing still.
Dizziness can also be a symptom of low blood sugar (hypoglycaemia), which can occur when blood glucose levels drop too low, particularly if diabetes medications are not taken as prescribed or if meals are skipped.
Additionally, dizziness can be a symptom of other diabetes-related conditions, such as nerve damage (neuropathy) or cardiovascular disease.
Can Diabetes Make You Tired?
Yes, fatigue is a common symptom of diabetes. It can result from high blood sugar levels and other diabetes complications, or be due to medication side effects. When blood glucose levels are too high, the body is not processing glucose as energy; therefore, tiredness or fatigue may occur.
Additionally, people with diabetes are at higher risk of developing sleep disorders such as sleep apnea, which may also contribute to feelings of fatigue during the day. However, fatigue is not always directly related to diabetes and can also have other causes.
Can Diabetes Cause Weight Gain?
Diabetes can cause both weight gain and weight loss. Insulin treatment for diabetes can sometimes cause weight gain, while diabetes-related conditions such as insulin resistance can also contribute to weight gain.
However, diabetes can also cause unintentional weight loss, particularly when blood sugar levels are consistently elevated, as well as due to other diabetes-related complications.
Diabetes: Where to Inject Insulin?
According to several reliable sources, there are several areas of the body where insulin can be injected. The preferred and most commonly used site for insulin injection is the abdomen, specifically the area around the navel. This is because the abdomen has a higher percentage of subcutaneous fat, which allows for more consistent and predictable insulin absorption.
Other sites that can be used for insulin injection include the upper arms, thighs, and buttocks. It’s important to rotate injection sites within the same area to avoid tissue damage, and to inject at least one inch away from the previous injection site.
Additionally, it’s recommended to avoid injecting insulin into muscle, as this can lead to quicker insulin action and a greater risk of low blood sugar. Before injecting insulin, it’s important to thoroughly clean the injection site with soap and water or rubbing alcohol, and to follow proper injection technique to ensure accurate dosing and minimize discomfort or complications. It’s also important to talk to your healthcare provider about the best injection sites and techniques for your individual needs.

Conclusion
In conclusion, diabetes is a chronic health condition that affects millions of people worldwide. It occurs due to a malfunction in the body’s ability to regulate blood sugar levels, either due to a lack of insulin production or poor insulin utilisation.
Diabetes can lead to severe health complications if left untreated, making early diagnosis and proper management essential. While Type 1 and Type 2 diabetes share some similarities, there are notable differences between the two conditions, and treatment options may differ depending on the type of diabetes. However, with a combination of lifestyle changes, medication, and regular blood sugar monitoring, it is possible to manage diabetes effectively and reduce the risk of complications, helping individuals live a healthy and fulfilling life.
If you are experiencing the symptoms of diabetes, it is crucial that you seek advice from your healthcare provider.
Please note: If you purchase products by clicking on links on this page, The Check Up may earn a small commission.
Personalised Nutrition for Diabetics
For many with diabetes, losing weight can be a beneficial step towards better health. But, figuring out the most suitable way to achieve this isn’t always straightforward. Everyone’s journey and challenges with nutrition and dieting are as distinct as their fingerprints.
Fortunately, whether you’re navigating the complexities of diabetes or simply want to improve your overall well-being, our diet matchmaking eBook offers a deeper understanding of personalised nutrition tailored for individuals like you.
What’s Inside:
- Recognizing 26 Challenges: Addressing common and unique hurdles individuals face on their weight loss journey.
- Exploring 11 Diet Plans: Uncover which method aligns best with your health goals and diabetes management.
- Interactive Diet Exploration: A tailored exercise to help pinpoint a nutritional approach suited to your needs.
- 2-Week Meal Plans for Each Diet: Begin your journey confidently with structured and easy-to-follow meal plans.
Over 200 pages of guidance available for just £3.99.
Your journey to better health shouldn’t be a generic template. Let our guide assist you in overcoming obstacles, whether you find challenges in emotional eating, need flexibility with cheat days, lack culinary skills, or face other unique barriers. With our eBook, find the tailored path that respects and supports your individuality.


